My left eye is target practice for the circus knife-thrower. The searing, white hot pain of his knives will eventually subside. The nausea, the vomiting, the isolation will pass; but the fear of the next attack remains.
This disease will not kill me, but is slowly steals my life. Migraine stops soccer games with my kids, dinner dates with my friends and stifles my once ambitious career. I have lost days, weeks, months, probably years of my life to migraine.
I have learnt to live with the agonising pain, but I cannot live with losing my life.
-Christine-
The World Health Organisation ranks migraine among the leading causes of disability worldwide. Migraine affects more people, than asthma, diabetes and epilepsy combined. Absenteeism through migraine, costs the Irish and British economies over £2.5 billion per annum.
These facts have fuelled funding into the science of headache; we now know more about migraine, and how to control it, than ever before. Learn how to decrease the frequency, duration and severity of your migraine attacks. Do not suffer needlessly.
Michelle Biggins
Chartered Physiotherapist
What is Migraine?
Migraine is a genetic, neurological, life-long condition. You inherit a brain capable of producing migraine, from your parents. Your migraine brain contains nerves that are better at producing headache than a non-migraine brain. Certain things, like stress and fatigue, make these nerves even more capable of producing headache. These kinds of things are called migraine triggers.
Every migraineur has a unique set of migraine triggers. Common triggers include; stress, fatigue, certain foods, skipped meals and neck pain. Migraine triggers, lower how well your body functions. A combination of migraine triggers, make you more susceptible to a migraine attack; similar to a person who gets a kidney infection, or cold, or back pain when they are run down.

How can Physiotherapy help Migraine?
1. Join forces with your GP
Your GP and physiotherapist will work with you to help you control your pain. If simple painkillers are inadequate, your GP may prescribe specialist migraine drugs called Triptans. There are many available, if one does not work; it can be worth trying another. The appropriate drug will enable you to control your pain during a migraine attack.
Using simple painkillers, >15 days per week (4 days/week), causes headaches. These are called rebound or medication overuse headaches. Simple painkillers include; Solpadeine, Panadol, Neurofen, anti-histamines and sinus tablets.
The number of days per month you take painkillers is the problem. The number of painkillers you take per day is relatively unimportant. Taking 1 painkiller per day, 15 days per month, will cause rebound headaches. Taking 4 painkillers per day, 6 days per month, will not cause rebound headaches.
Your GP may discuss preventative medication which you take every day. These drugs will not cause rebound headache. You should consider preventative medication if you get more than 15 headache days per month or migraine greatly disturbs your quality of life.
2. Find your migraine triggers
Identifying your migraine triggers is essential to migraine management. A migraine diary tracks the number of headaches per month, their severity and duration, and painkiller usage. A diary illustrates migraine patterns and highlights your triggers. Download a free migraine diary from Migraine Ireland or Migraine Trust
Some migraine triggers are things you do every day; poor sleep patterns, irregular diet, reaction to stress. It is hard to change your daily habits. Many physiotherapists have training in Cognitive Behavioural Therapy. CBT techniques teach you how to make gradual changes to your routine. Changing your daily habits will decrease your migraine triggers.
↓ Migraine Triggers = ↓ Headaches
3. Exercise Vs migraine drugs
It is impossible to exercise during a migraine attack and 20% of people report exercise as a trigger. However, when exercise is properly prescribed for migraine, it can be used as a preventative drug.
Swedish researchers compared 40 minutes of exercise, 3 times per week, to the leading migraine preventative drug Topirimate. This innovative study proved exercise equalled Topirimate, giving patients a greater number of headache-free days per month. Side effects of exercise include; weight-loss, improved sleep, reduced anxiety, increased energy and decreased risk of heart disease and stroke.
4. Neck pain and migraine
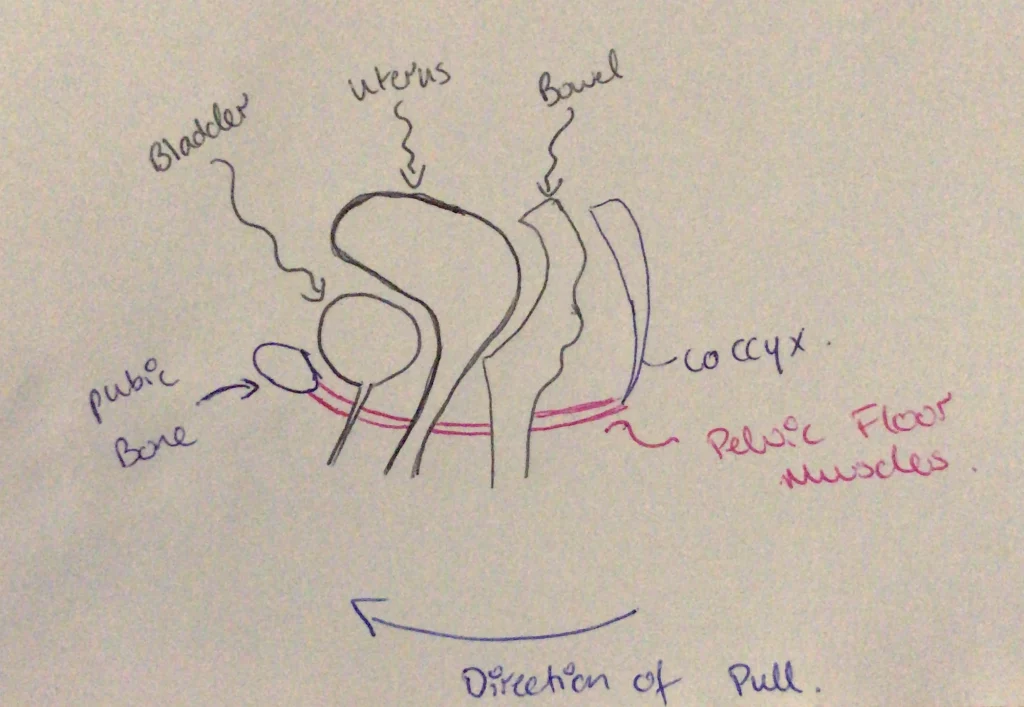
Neck pain can either be a migraine trigger or a migraine symptom. A trained physiotherapist will diagnose if your neck pain is a migraine trigger or not.
Physiotherapy for neck pain and headache aims to reduce the pain that muscles, joints and nerves refer into the head. Treatment options include manual therapy, dry needling, trigger point release and massage. Exercises will decrease pain referral from muscles, joints and nerves into the head.
↓Neck pain as migraine trigger = ↓ Headaches
Where can I access physiotherapy for my migraine?
Physiotherapy clinics in Ireland can be found on www.iscp.ie. Your GP can also refer you to one of the five specialist migraine centres in the country www.migraine.ie/specialist-clinics.
Take home message
We know more about migraine than ever before
Finding the right drug is crucial for a migraine attack
Simple painkillers, for more than 15 days per month, cause headaches
Exercise is one of the top preventative migraine drugs
Controlling your triggers controls your migraine
Neck pain can be a migraine trigger
Stay informed, new research into headache and migraine is ongoing
Michelle Biggins is chartered physiotherapist with a special interest in headache and migraine. Her post-graduate training in headache and migraine has taken her to Curtin University in Perth, Royal College of Physicians in London, and Beaumont hospital in Dublin.
She runs a headache clinic in Oranmore, Galway and is available for appointment on 0353851670574 or info@proactivephysio.ie. If you are interested in headache and migraine, sign up to our FREE monthly newsletter located in the top right hand corner of this page.
References:
1. European Headache Federation (2007) WHO: Lifting the burden: The Global Campaign to reduce the burden of Headache Worldwide. Aids for Management of common headache disorders in primary care J Headache Pain 8:S1 DOI 10.1007/s1094-0007-0366-y
2. The International Classification of Headache Disorders 2nd Ed. (2004) Cephalalgia Vol 24 Supple 1
3. Headache Disorders-not respected, not resourced (2008-2009) A report of the All-Party Parliamentary Group on Primary Headache Disorders (APPGPHD) House of Commons Report
4. Negro & Martelletti (2011) Chronic Migraine plus medication overuse headache: two entities or not? J Headache Pain 12(4): 593-601
5. Varkey et al (2011) Exercise as migraine prophylaxis: A randomised study using relaxation and topiramate as controls Cephalalgia 31(14) 1428-1438
6. Baillie et al (2014) A systematic review of behavioural headache interventions with an aerobic exercise component Headache 54: 40-53
7. Goadsby & Akerman (2011) The trigeminovascular system does not require a peripheral sensory input to be activated-migraine is a central disorder Cephalalgia 32(1)3-5
8. American Headache Society www.americanheadachesociety.org
9. International Headache Society www.ihs-headache.org
10. World Headache Alliance www.w-h-a.org
11. European Headache Federation www.ehf-org.org
12. British Association for the Study of Headache www.bash.org.uk
13. Migraine Association of Ireland www.migraine.ie
14. National Migraine Centre UK www.migraineclinic.org